It has been 24 centuries since Hippocrates, known as the father of Medicine, pronounced the aphorism of “Desperate diseases must have desperate remedies”. Today, in 2020, we could not agree more.
The urgency of the health situation caused by the irruption of SARS-CoV-2 in our lives has accelerated the research processes and has focused all (or almost all) the scientific-technical efforts of the last months into the development of a vaccine for the famous COVID-19 in an unprecedented way.
In December 2020, almost a year after the origin of all this crisis, it seems that we finally see the light at the end of the tunnel and the news about a safe and effective vaccine has ceased to be a socio-sanitary dream to become a reality discussed in the news day in and day out.
But how do these vaccines (in which we have placed so much hope) work?
COVID-19 vaccines: a new method
Everything around this pandemic is new: the situation, the crisis and even normality, so the vaccines could not be less. Currently, the two main bets on the market (Pfeizer-BioNTech and Moderna vaccines) contain a molecule never before used in vaccines: messenger RNA.
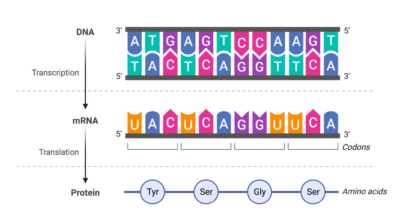
Viruses take advantage of their host to form themselves, and with these types of vaccines we have turned the tables. Let me explain: when a virus infects a cell, it sends a template (in the form of mRNA) to the cellular machinery, so that it builds the proteins that the virus needs to be able to infect more cells. That is, a kind of Trojan Horse, but in a very reduced version.
mRNA vaccines, mimicking the mechanisms of viruses, exploit the host’s cellular machinery to produce viral proteins, which will generate immunity.
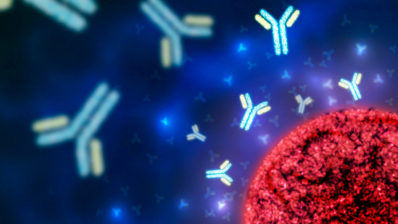
Thus, the vaccines that have already begun to be administered, consist of a synthetic mRNA that simulates the viral one. Once in the cell, it will cause the creation of some of these viral proteins. By recognizing them as external (and therefore as a threat), our body will react and will generate immunity. But these proteins won’t be able to cause disease because they are isolated, that is, without any virus that can use them.
Therefore, by exposing our body to viral proteins, we will be generating a preventive immune response (as if it were a simulation), which would protect us against a future and hypothetical entry of the virus into our body. Thus, in the event that the virus were to enter, although it would be doing so for the first time, the “Wanted” signs would already be hanging since long ago.
Learning to fish pathogens
Who hasn’t heard the saying “Give a man a fish and you feed him for a day. Teach a man to fish and you feed him for a lifetime”? Well, if we make a parallel with our body, a medicine that protects us in a timely manner would be the fish that takes away our hunger once, while vaccines would be learning to fish.
Although the messenger RNA method is novel because of the bait used (continuing with the analogy), the type of immunity it generates is the same as the more traditional vaccine models, since they are all based on the same concept: preparing our body to recognize a pathogen and attack it when it enters.
The other types of vaccines traditionally used are:
- Attenuated: they use a living but weakened form of the pathogen that causes the disease. The immune response they generate is very effective, since the infection is very similar to the natural one.
Measles, mumps, or rubella.
- Inactivated: they use a dead form of the pathogen. As a consequence, the immune response they generate is less durable than with living forms, but they are safer.
Hepatitis A, flu
- Subunit: parts of the pathogen are introduced, such as specific proteins or sugars. The response may not be as efficient as the previous ones.
Hepatitis B, Human Papillomavirus
- Toxoid: they include toxins, so they immunize against the effects of these, not against the entry of the pathogen. They are a type of vaccines that only apply to diseases caused by toxins, and therefore, not applicable in the COVID-19 situation.
Diphtheria, tetanus
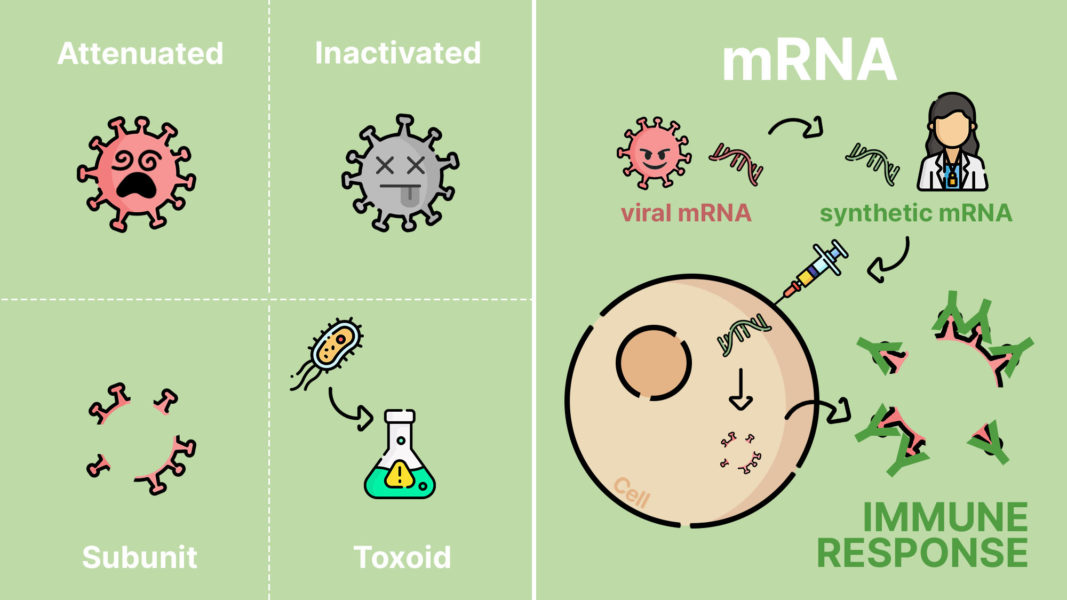
Why mRNA?
Now that we know the differences (and the similarities) between the different vaccines, what are the pros and cons of using mRNA vaccines compared to the more traditional ones to fight against SARS-CoV-2?
The negative aspects of these vaccines are not related with the short time in which they have been developed, nor to their safety, since they have followed all the usual protocols. However, two weak points should be noted:
- The uncertainty of the new (squared): In addition to being the first mRNA vaccines, we must add that we are dealing with a virus that we have not quite mastered. Thus, these vaccines may not provide us with as long-lasting or effective protection as other more established ones against better known pathogens and with more proven methods. Even so, the results of Pfizer and Moderna show effectiveness of more than 90%: totally hopeful results.
- Maintenance difficulty: To prevent the mRNA from being degraded by enzymes, keeping the contents of the vaccines at low temperatures is essential. Furthermore, to facilitate transport into the cell, the mRNA has to be covered by lipid nanoparticles (that is, fat) that are much more stable the more solid and colder they are, like butter in the fridge.
As for the positive aspects, they are fundamentally related to the logistics of the supply:
- Ease of production: obtaining the mRNA is simpler than the production of the virus’ own proteins or the attenuated or inactivated variants of the pathogens, so the production process would be facilitated.
Furthermore, given that the method takes advantage of our cells’ own mechanisms to generate viral proteins, the time required for the creation of vaccines is shortened. This way, vaccines should be easily and rapidly distributed on a large scale.
- More powerful response: due to its biological characteristics, mRNA triggers a stronger and more complex immune response than other types of vaccines, activating the entire immune system without the need to add other components to vaccines, as is normally done in other types.
- Safety: by not introducing the virus in any of its forms (neither attenuated nor inactivated), there would be no possibility of developing COVID-19 from the vaccine.
Light at the end of the tunnel
As Hippocrates’ idea exposed, a situation as critical as the one we are experiencing has pushed the scientific community to the limit, which has made a race against time to find a vaccine.
Now that we have it, the short time in which it has been achieved seems to generate doubts in many people, but – what would happen if only two people ran in a marathon? The answer is simple; possibly, none will reach the end, because doing so is not at all easy. However, if thousands of runners are put on the track, the chances of someone reaching the goal will be much higher. In this case the same has happened, and the injection of money, effort and interest on the part of companies, governments and institutions has allowed us to do the unthinkable (but not impossible!).
For months, society has been demanding measures to face this health crisis and it seems that at last some solution is arriving in the form of a vaccine. Now is the time to respond, collectively and above all individually, with the trust that the scientific community deserves. It is the time to thank the effort, and not only by clapping. It is time to continue with the precautionary measures and, when it is our turn, to get vaccinated.