Isabelle Thierry Chef (14 July 1972) is a chemist by training, currently working as an epidemiologist. Currently the Head of the Medical Radiation Group at the Barcelona Institute for Global Health (ISGlobal) – and an avid flamenco lover! -, she tells us about her scientific career so far and about what it takes to be a researcher.
You studied chemistry; how did you end up working on epidemiology?
My ‘chemistry life’ was more than 20 years ago… I hardly remember it now! I studied chemistry in Lyon, but already during my master’s degree in Marseille, I met Elisabeth Cardis – now head of the radiation program here at ISGlobal – and started to be interested in radiation protection and in applying it to health and society. After a second Master in Strasbourg (France), I started with my PhD. Since then, I have always been between the technical and the epidemiological aspects of radiation protection.
“I have always been between the technical and the epidemiological aspects of radiation protection”
What type of projects have you been working on?
I did my PhD on radiation protection with Elisabeth Cardis when she was at IARC (International Agency for Research on Cancer)in Lyon. The aim of the PhD was to analyse the exposure of nuclear workers, as part of a very large epidemiological cohort that was set-up by Elisabeth and partners from 15 countries. My PhD was on reconstructing the doses that the workers have received in their career and on quantifying the uncertainties on the doses recorded by the badges (dosimeters) that workers were wearing, mainly those used in the past. Since this was a cohort of workers who started working on the 1940’s, my task was to assess the type of badges that were used over time and to compare the technologies of the badges that were used in the past and nowadays.
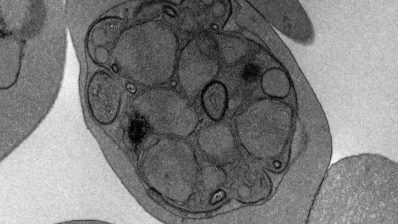
After my PhD I got interested in medical exposures, so I moved to Paris and I worked at the IRSN – Institut de Radioprotection et de Sûreté Nucléaire to study the exposure of premature babies in intensive care. In premature babies, the respiratory and digestive system are still under development after birth so radiographs are taken every day or two for surveillance of respiratory and digestive conditions of preterm babies. Because premature babies are very sensitive and fragile we wanted to make sure that their exposure to radiation remain at low doses and would not be detrimental for them. We concluded that the doses were really very low and we didn´t pursue in following the population. That was my first project in medical exposures focusing on children. Since then it has been building one step after the other, and in my group here in ISGlobal I am still focusing on studying medical exposure.
Always with children?
Yes, I’d say paediatrics is my major concern, although I’ve also done some studies in adults, for example on doses from mammography … But I want to emphasize that the medical and radiology community, especially in the paediatric field, are in general aware of the risks associated to the use of ionizing radiation, and they are relatively careful in keeping them as low as possible … And it is also important to emphasize that Low dose, Low risk!
“The medical and radiology community are generally aware of the risks associated to the use of ionizing radiation, and they tend to be careful in keeping them as low as possible”
After Paris you then went to the US… what did you do there?
I did a postdoc at the NCI (National Cancer Institute) for 2 years. At NCI I continued working on the topic of medical exposure and I did some exposure assessment on the brain of children treated by interventional radiology, that is, when X-ray is used to guide small instruments such as catheters through blood vessels so that treatment is performed without surgery. In our study, we considered procedures performed in the brain of a cohort of less than 50 children, quite small because it is a rare procedure.
When I came back from the US, I joined Elisabeth Cardis at IARC (once more) and we started the implementation of a very large project, on which we are still working: the EPI-CT Study, a European cohort with 1 million children who have been involved in CT scanning. The majority of the cohort will be followed as part of a large European Consortium (MEDIRAD) to further investigate the impact of CT scanning on the pediatric population.
“I am coordinating a new project, HARMONIC, where we will build a large cohort of 100,000 children involved in cardiac interventional procedures”
Medical exposure in children is a topic that we are going to further explore here with the new HARMONIC project, which has just been accepted for funding by the European Commission and which I am coordinating at ISGlobal. The project involves, on the one hand, building a large cohort of children involved in cardiac interventional procedures. In epidemiology you need a decent size of a cohort to draw conclusions, and in our case, we aim to include 100,000 children treated for heart defects.
One of the strengths of this project is that we involved medical doctors from the very beginning. Traditionally, I have been involved in retrospective data collection, looking at old files and archives… In HARMONIC, we are anticipating prospective data collection, including blood sample for biomarker investigations and direct contact with patients. We therefore need a strong collaboration with medical doctors because they are the ones who will have direct contact and maintain the relationship with the patients.
What other projects are you involved in at the moment?
Another topic of the HARMONIC project is modern radiotherapy including proton therapy, a new radiotherapy technique, that is little by little used on children mainly for the treatment of brain tumors. The use of protons instead of photons (as in conventional radiotherapy) allows more precise delivery of doses to the tumor with less impact on surrounding tissues. In this context, we aim at building a large cohort of pediatric cancer patients to initiate a pan-European registry.
“The use of protons (proton therapy) instead of photons (conventional radiotherapy) allows more precise delivery of doses to the tumor with less impact on surrounding tissues”
What kind of effects are you looking for?
We look mostly at cancer as the principal side effect of radiation. Depending on the type of cancer it can develop a long time after the radiation. The fastest cases can appear between 2 to 5 years after exposure, but normally we’re talking about decades. This is the reason why we usually work retrospectively. Nowadays, with the electronic systems collection of data is easier, although we do have to go back to the paper files sometimes…
How does the research funding system affect these long-term projects?
It’s tricky, because most grants run for only 5 years or so… So you have to plan very well when is the time to reopen a cohort, maybe every 5 to 10 years. This is what we did with the nuclear workers studies, we published the first results in 2005-2007 and restarted with the follow-up of part of the cohort (INWORKS) in 2010. By the time the project starts, you do the work and publish it, it is already time to ask for a new grant and start again!
How has been your experience of working in different countries?
I always think it’s the people you work with that makes the difference; if you have a good team, working is always nice. I have to say I am quite lucky because I managed to keep strong relationships with people from my former groups and we still continue working together on some projects..
“It’s the people you work with that makes the difference”
What are the biggest challenges in research and your field particularly?
The funding is always a challenge, whatever the field, I think! And ethical issues are essential when you are working with human beings. You have to work hard to ensure that your ethical issues are being taken care of – this ‘ethical clearance’ is actually a specific part of the projects, now. Working with international cohorts with patients from different countries and different laws is therefore complicated.
What’s the most important trait for a scientist?
Patience.
What do you like most about doing research?
What I like the most is really the international set-up and the collaborations that we have, working with people from everywhere.
And the worst thing about science?
I’d say, also patience! Sometimes you want the projects to be finished and published but they have long duration and you have to be patient.