Jordi García-Ojalvo is the director of the Dynamic Systems Biology Laboratory of the Department of Experimental and Health Sciences, Pompeu Fabra University (DCEXS-UPF) and his group is part of an interdisciplinary project that aims to apply technological innovation to neuroscience: Neurotwin.
The project has brought together experts from very diverse branches such as engineering, clinical research and philosophy, to create “digital twin brains” that allow personalized treatments for neurological diseases.
We have talked with Jordi García-Ojalvo to better understand this interesting project.
“Digital twin brains” sounds like science fiction… What is the project about?
The Neurotwin project is the successor to an initiative that encompasses many projects called Virtual Physiological Human, which was based on the idea of creating a complete model of a human being on a computer, to perform non-invasive tests at the computational level. Now the concept has evolved to “Digital Twin”, which seeks not only to have a single computational model for everyone, but to create “twin” digital models of each patient to be able to make personalized medicine from the genome of each individual.
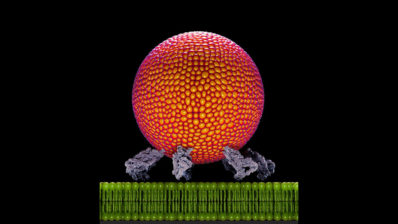
Specifically, in our project, Neurotwin, we have focused on digital twin brains, which are representations of patient brains created from data extracted with current neuroimaging and brain activity monitoring techniques.
What is the utility of these “neuro twins”, then?
The purpose behind the creation of these models is twofold:
- On the one hand we want to try to understand why non-invasive brain stimulation treatments with electric or magnetic fields work. They are currently already used to treat neurological and neurodegenerative disorders with success, but we don’t understand how or why they work.
- Once this is achieved, with detailed models of the brain, we will be able to answer different questions about the treatments and make in silico modifications so that they have maximum effectiveness for the general population and, ideally, for each patient.
“We know that non-invasive brain stimulation treatments with electric or magnetic fields work, but we are not completely sure about why”
And specifically, with what diseases could they be used?
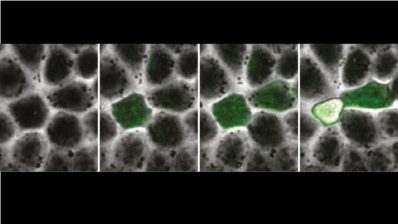
We are focused on Alzheimer’s because the entities with whom we collaborate are working with patients with this disease. What has been seen in Alzheimer’s, for example, is that there are disturbances in the oscillations and rhythms of the brain. With these magnetic and electrical stimulation techniques, if we could modulate the oscillations and reproduce the rhythms of a healthy brain, perhaps we could reduce the symptoms in mild stages of the disease, or its progression.
“If we could modulate the oscillations and reproduce the rhythms of a healthy brain, perhaps we could reduce the symptoms in mild stages of Alzheimer’s”
Even so, once the project is validated, these types of techniques could also be translated and transferred to patients with depression, epilepsy or different types of dementia.
Who else is participating in the project?
This is a project coordinated by the Neuroelectrics Barcelona company and supported by the EIC Pathfinder Horizon 2020 of the European Union, which is an initiative to support the research and development of cutting-edge technologies.
Thus, in the project there are experimental and theoretical groups:
- Among the experimentals, a group from the Pablo de Olivade University in Seville works with mice and three groups work with humans: one in Dortmund (Germany), another in Italy and another in Boston, at the Beth Israel Deaconess Medical Center, where they work with Alzheimer’s patients.
- Regarding the theoretical branch of the project, both we and Gustavo Deco’s group (UPF) are dedicated to computational models and the analysis of patient data.
And what will the work dynamics be like? Have you already started?
The project started a few months ago, yes, and it has a duration of four years. In the first steps we, theoretical and computational researchers, will try to develop models to understand how these non-invasive stimulations work and optimize them for future application to patients, which would be the second part of the project.
“Theoretical scientists can begin to work with data that already exist and then add the information that the experimental personnel, who are starting to work with the patients, send us”
Once the models are developed, they will have to be validated. Later, we would like to make these models usable in general, not just for research, and thus be able to apply them in the clinic in a personalized way.
How would the process to generate a personalized model of a patient be?
Ideally, both structural and functional data from the brain are needed. The structure’s data can be obtained with a magnetic resonance imaging (MRI) and with a technique called Diffussion Tract Imaging (DTI) that allows to measure the level of connectivity between different areas of the brain, but also from existing data.
Once we have the structure analyzed, we must obtain data on its functioning, that is, how the brain behaves. This information can be obtained with data from electroencephalography, which shows activity levels over time, or from functional magnetic resonance imaging, which are the typical images that show how the brain “lights up” as we stimulate it with different inputs.
With all these structural and functional data, mathematical models that describe how the different neuronal populations connect with each other, would allow us to generate the computational models, the Neuro Twins.
“Making these models is not complicated at the conceptual level, because we believe that we know the mathematical laws (or at least we have a good approximation) and we have the tools to obtain the experimental data”
At a hypothetical level, in clinical practice, the process of generating a personalized model would not be too expensive or too slow: in the same session we could obtain an MRI and ITD of the patient (structure) and in another session the functional MRI ( activity). Therefore, in a couple of days or at most a week and in a non-invasive way, we could have the necessary data of the patient.
So, when will we be able to talk about personalized neuromodulation at the clinical level?
We have the goal of doing it by the end of the project, so we are talking at least four years. In order to do it, though, we don’t depend on new technologies so we don’t have a too distant horizon; in a few years it could be established.
In addition, if new techniques to obtain information from the brain were developed, we could incorporate them into our models to enrich them, but it would not make us go back.
Let’s get a little philosophical to finish… Do you think that one day we will be able to represent a complete brain in a computer, thoughts included?
Right now at the computational level we cannot represent the complexity of the brain, which is a marvel – it has a negligible energy consumption for the amount of information processing it does! – and partly also a mystery. But to do personalized medicine it is not necessary (nor does it make sense) to try to represent and modulate a brain down to the microscopic scale.
Now, if we talk about including thoughts, we are already entering the world of artificial intelligence and therefore we would have to forget about a 100% faithful representation. That is, if we do an abstraction exercise, perhaps we could generate an artificial model that would do something similar to thinking… But whether that would be representative of what the human brain does, I am not sure.