The biologist and sports enthusiast, Toni Celià-Terrassa (Sa Pobla, Mallorca, 1982), is currently leading the Cancer Stem Cells and Metastasis Lab at the Hospital del Mar Medical Research Institute (IMIM) since January 2018. Here he studies how breast cancer cells transform into malignant cells and metastasize to other organs.
What and where did you study?
I studied a double degree in biology and biochemistry at the University of the Balearic Islands (UIB), in Mallorca. In my last year as an undergraduate, I worked in the summer at the CNIC, in Madrid. There I had the opportunity to carry out my PhD in a laboratory in Barcelona, at the IBMB-CSIC. We worked in metastasis, and I totally knew that this was the subject in which I was interested.
Why this interest in metastasis?
Because at the biological level it is a very complex and interesting process. Cells must do really extraordinary things to metastasize… They need super-powers! But most importantly, because of the relevance that it can have on a clinical and social level. More than 90% of cancer deaths are due to metastasis, not because of the tumor in situ.
“Cancer cells must do really extraordinary things to metastasize… They need super-powers! It makes them a fascinating system to study.”
Where did you go next?
During my PhD I went to Princeton for four months, and they offered me to come back as soon as I finished, in order to do a postdoc there. It was a very good laboratory, led by Yibin Kang, one of the pioneers in metastasis organotropism, that is, the fact that each type of cancer affects a different type of organ when it metastasizes. So I didn’t hesitate. In Princeton I studied breast cancer, cancer stem cells, primary tumors and metastases and EMT…
EMT?
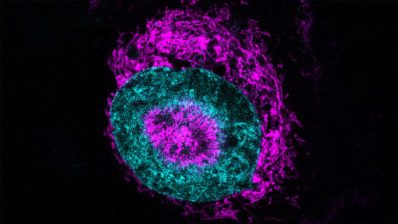
Epithelial-mesenchymal transition. It is a process whereby epithelial cells become another cell type, specifically mesenchymal cells, which are more mobile and invasive. It is a process that must happen for metastasis to occur, but it must also be reversible for the tumor to grow later. In fact, it was in the IMIM where EMT – a program that was by then known as essential in embryonic development – was discovered to be also involved in the first step of metastasis. It was in 2000, in the group of Antonio Garcia de Herreros in the IMIM, as well as in Ángela Nieto’s research group in Madrid. Since then, there has been a “boom” in this field…
And you came back to Barcelona.
Yes, in Princeton I learned a lot but, after 5 and a half years, I knew I wanted to come back home. In fact, at that time I was thinking of quiting research if I didn’t get a position here in Barcelona…
Luckily, you got it!
Yes, in 2017 they gave me a Miguel Servet scholarship, and in January 2018 I joined the IMIM and created my group, starting from scratch.
How was the experience?
It is very motivating and exciting to create a group where you can follow your own lines of research. It is a very exciting challenge. But it cannot be denied that it also involves many difficulties and a lot of uncertainty… Especially in terms of obtaining funding, which can be a matter of luck. And I actually have been very lucky, because I have received funding from various sources, and this has allowed me to have a large research group composed by six people.
“Starting your own group is very motivating and exciting, but it also involves many difficulties and a lot of uncertainty, especially in terms of funding“
And you are still studying breast cancer metastasis… And, now, immunotherapy as well.
We focus primarily on the evolution of tumors, and specifically on the development of metastasis. Not on how the primary tumor cells escape, but how and why they get to settle in another place. Experiments have shown that there are millions of cells that escape from a primary tumor, but only 0.1% of these cells are capable of creating a secondary tumor. We want to understand what is special about these cells, especially in their interaction with the immune system.
There are millions of cells that escape from a primary tumor, but only 0.1% of these are capable of creating a secondary tumor.
Are we moving forward in the therapeutic application of immunotherapy?
There are different types of immunotherapy that are being tested, like the CAR-T or the blockers of the immune system control points (immune check points), which is the most successful type.
This year, 2019, the first immunotherapy treatment for metastatic triple negative breast cancer has been approved. This is the breast cancer with the worst prognosis, and now this treatment can be used in the clinic! In melanoma and lung cancers, immunotherapy has been used since some years ago, and when it works (perhaps in 20-40% of cases), it works very well and in the long term. The problem is when it doesn’t work… A lot of research is focused onn this field right now!
Have you ever thought about leaving science?
Yes! While I was doing my postdoc, I thought about it several times! It is a difficult phase because you are in a professional limbo… In the lab I was working on that time I had the best resources, so there was a lot of pressure to do it very well. Doing it just “well” is not enough.
What is the hardest part of research?
The fact that you must be continuously in search of funding; you spend more time doing that than on research! Grants are short, there is no continuity and not enough money… In the US, almost 3% of the GDP is dedicated to research, while here in Spain we only dedicate 1.2%… Some associations such as ASEICA or AECC and others, are currently proposing a national R&D plan to increase the investment up to the European average, around 2%.
Research is a perverse system because even if you are very good at your job, it is not enough! The ‘luck’ factor is important, even when receiving funding. There is a lot of pressure because a stroke of bad luck – a failed grant – can block you.
And the best part?
On a practical level, when you have an intuition or groundbreaking idea and it is confirmed experimentally. On a global level, seeing how your discoveries can have a social impact, in our case, on patients.