According to the World Health Organization, more than 70% of drug-related deaths are associated with opiates, of which 30% are caused by overdoses. This is because these types of drugs, key to the treatment of chronic or neuropathic pain, generate great dependence and addiction in patients.
Now, a project led by researchers from the Department of Experimental and Health Sciences, Pompeu Fabra University (DCEXS-UPF) Rafael Maldonado and David Andreu has found an alternative: co-administering THC, the psychoactive component of cannabis, together with a peptide they have developed that avoids the side effects of this substance.
This combination of drugs could become the first treatment approved by the EMA / FDA for chronic pain. We spoke with David Andreu, head of the Proteomics and Protein Chemistry Unit at DCEXS-UPF, to tell us more about this success story.
Where does this project come from?
The goal arises from the need to find a treatment for chronic pain that is more effective than the existing painkillers for mild pain such as ibuprofen or paracetamol, and which does not cause addiction, as happens with opiates. In this sense, cannabis opens a therapeutic window in the middle of these two pathways, each of them problematic on its own.
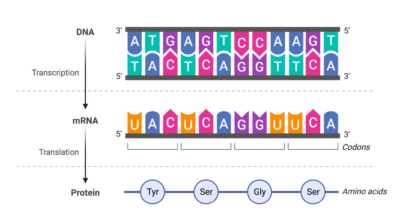
The idea is based on previous work by the group of Rafael Maldonado and external collaborators who discovered a cross-talk, an interaction between the cannabinoid receptor and the serotonin receptor of the nervous system. Both receptors are activated by THC so that when cannabis is consumed, analgesia is achieved but it comes with undesirable side effects in terms of memory and other cognitive functions.
Based on this information, they hypothesized that blocking the cross-talk between the cannabinoid and serotonin receptors could maintain analgesia yet minimize side effects. This could be initially achieved by some peptides, but they were totally undruggable, i.e. unviable as drugs. This is when our team joined the project.
So what has been your role?
Basically what we have done is find a way to make these peptides druggable, that is, to turn them into a drug. This is not easy in general, and for peptides it can be especially tricky.
In this particular case, the challenges were many: to transform a peptide with many initial limitations into a magic bullet that meets the conditions the pharma industry wants to find in a drug for the central nervous system (CNS): to be able to cross the blood-brain barrier, to be stable in a physiological environment (the Achilles heel of many peptides!), not to be immunogenic and, the icing on the cake, to be orally active.
“Getting a peptide from undruggable to druggable is easy to say but hard to do”
To achieve this, we have used the most current versions of the rules of medicinal peptide chemistry that years of practice in this field have taught us to apply creatively, but which are a bit complicated to explain here.
Briefly, performing in silico molecular dynamics simulations and then applying criteria of medicinal peptide chemistry we have been able to access (that is design, synthesize and test in vitro and in vivo) a series of candidates increasingly effective in overcoming the challenges I was talking about before.
It is important to emphasize that both activities (in silico and chemical studies) complement each other: in silico tools are undoubtedly valuable, but we must not lose sight of the fact that the development of a drug still involves further in depth research, and remains a fundamentally experimental process with an essentially empirical component.
“For the development of this peptide we have used the entire catalog of tools for peptide medicinal chemistry, in many rounds of trial and error.”

So your work is already finished or will you continue to move forward with the project?
The UPF and the other institutions in the consortium share the intellectual property of the drug and its application. In fact, the patented product is difficult to improve; as I said, the main obstacles to development have already been overcome, so this intellectual property is the main asset of a spin-off that UPF Ventures is driving to continue developing the project.
“The product we have developed is already highly optimized and is difficult to improve pharmacologically”
Right now we are completing the preclinical phases, with trials in mice for the treatment of different types of pain (chronic pain, neuropathic pain, osteoarthritic pain), and at the same time trying to capture more funding.
And what do you think of the stigmas surrounding the medicinal uses of cannabis? Do you think that at some point this has limited you, for example in getting funding?
For now it is not being a determining factor, but it is true that enthusiasm is limited in the most stablished sectors of the pharma world. The issue is controversial; on the one hand there are sectors eager to take advantage of this intermediate route for the treatment of pain, but on the other hand there are also other influential sectors (including well-established pharma companies), rather reluctant to the medicinal use of cannabis. Both fields have respectable arguments.
What is clear is that cannabis use so far has adverse cognitive effects, but our proposal to administer THC (in pharmaceutically regulated versions) in conjunction with our drug, could give patients very satisfactory levels of analgesia without the side effects of this substance or the risk of addiction generated by opiates.
You must be happy with the results!
On a personal level, the development of this project has coincided with my coming back after a difficult period, so I am very pleased with what we have achieved.
It has not been an easy task and we would be excited to see it become a practical reality.
Hear David Andreu and his colleagues talk about this project in this video (in Catalan).
Gallo M et al. Orally Active Peptide Vector Allows Using Cannabis to Fight Pain While Avoiding Side Effects. Journal of Medicinal Chemistry, 2021