Rafa Vilasanjuan is director of the Global Analysis and Development Department of the Barcelona Institute of Global Health (ISGlobal), and a member of the GAVI (The Vaccine Alliance) Civil Society Steering Committee, where he is also involved in the CovaxFacility platform.
The CovaxFacility is an international initiative of GAVI, WHO and the Coalition for Epidemic Preparedness Innovations (CEPI) that aims to accelerate the development and production of COVID-19 vaccines, guaranteeing a fair and equitable access for all countries in the world.
We spoke with him about the ongoing vaccines against Covid19, and how we have to consider their worldwide distribution to end this global pandemic.
How many vaccines are currently being developed?
Right now there are about 200 vaccines being tested, but only about 10 are in phase II or III of the clinical trials. It must be taken into account, however, that only 20% of those that reach clinical trials (or 50% of those that reach phase III) end up being approved. So we can say that by 2021 we will already have 2-3 vaccines for distribution.
What type of vaccines are they?
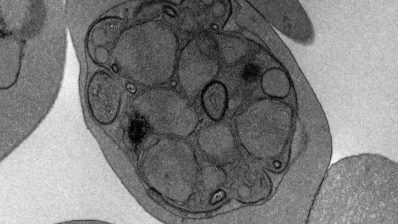
Different types of vaccines are being developed, including for the first time, mRNA vaccines, where instead of introducing the inactivated virus, only its genetic material is used. They are easier to produce, but more difficult to develop.
“By 2021 we will probably have 2-3 vaccines for distribution”
How can the development be that fast?
On the one hand, more resources are being put in than ever before, and this speeds up the process a lot.
On the other hand, processes are being shortened, and some that normally take place one after the other, are now being done in parallel. Some examples of these ‘shortcuts’ are:
- Merging of phases II and III of clinical trials
- Creating vaccine production plants before having the vaccine: the biosafety conditions are different for each vaccine, and that is why specific production plants are needed, which are normally built once the vaccine is already available. What some countries are doing now, such as the United States with the “Warp speed” operation, is to start creating production plants before having the vaccine.
- Producing the vaccine before its approval: some pharmaceutical companies have already said that, since the ‘factories’ will be already created, as soon as there is evidence of the safety and efficiency of the vaccine, they will begin to produce it, without waiting for it to be licensed – something that can normally take months or years!
So factories will be built and vaccines will be produced without knowing if they will come out … Both points are a giant investment at risk, because these vaccines might end up being useless!
Will this speed affect the efficacy and safety of the vaccines?
If done right, safety doesn’t have to be compromised. Although regulatory bodies are also reducing the time they require to consider a vaccine safe and efficient, it is clear that safety has to be 100% well documented.
Efficacy is different. Normally, for vaccines a degree of efficiency of 60-70% is required. But due to the emergency situation, a 40-50% effectiveness might be enough for now.
“Normally, for vaccines, a degree of efficiency of 60-70% is required. But due to the emergency situation, a 40-50% effectiveness might be enough for now.”
So, vaccines will be approved earlier and being less effective?
There are several types of regulation of vaccines by official international organizations:
- Total regulation: it requires a lot of time to be able to see all the possible effects. For a new vaccine it would take about 2-3 years after finishing all the trials. In the case of SARS-Cov-2, since there is already a lot of approved research on SARS and many of the vaccines are derived from these, it could take 6-8 months, or some say even just 2 months, to have a dossier of regulation approved.
- Regulation based on emergency: it consists of applying doses of vaccines to a target population (for example, medical staff) just after the trials, that is, temporarily shortening the regulation process. The US and the UK have already said they will do so; we still don’t know what Europe will do.
With all that is being done – creating plants before having a vaccine, producing the vaccine before having official approval – the process of developing a vaccine is being shortened from 10 years to 18 months!
“The process of developing a vaccine is being shortened from 10 years to 18 months”
When could we say that we will have a vaccine?
We are hearing a lot that there are some vaccines already, or that we will have them by the end of the year… Actually they talk about having vaccines for clinical trials. But we can only consider that we have a vaccine when it is regulated for everyone. Not in clinical trials or just emergency regulated.
And how will it be distributed?
This is a sensitive and very important topic. Right now, worldwide we have capacity to generate around 2,000 million annual doses of the Covid19 vaccine. AstraZeneca has already committed 1 billion doses of the Oxford vaccine in one year – and in fact for the first time in history they have already been sold, before the vaccine has been produced and even before knowing whether it will exist! They have sold 300 million to the European Union, 300 million to the Covax platform, 300 million to the US, and 50 million to Great Britain.
“For the first time in history vaccine doses have already been sold, before the vaccine has been produced and even before knowing whether it will exist!”
But of these 1 or 2 billions, who should receive the first doses?
We must ensure an equitable distribution among the countries, because it is useless that we all have the vaccine here if, for example, in Morocco or Latin America they don’t get the vaccine. We would have to close borders. Because we must remember that the fact that we are all vaccinated does not mean that we are all immune – we have said that the efficacy will be 50%, so half of us will still be susceptible! For this reason, it is better to vaccinate 20% of the population of each country, than vaccinating 100% in Spain, for example, and nobody in Morocco.
“To control the epidemic and restore economic, social and work stability throughout the world, the vaccine must be distributed fairly, for example by vaccinating 20% of the population of each country”
Is that what the Covax platform proposes?
What this international platform proposes is to ensure vaccines to cover 20% of the population of each country, following certain criteria to decide how to distribute the first vaccines among this 20%, such as the percentage of the population, the peak of the epidemic, risk sectors… and always keeping one part for emergencies. This clashes head-on with the interests of the states, who want to ensure vaccines for their populations. That is why CovaxFacility accepts that the richest countries produce more doses for themselves, but provided that they contribute to finance the 20% of the countries that do not have the capacity to make agreements individually.
And there are still many other open fronts…
Sure! I have been doing daily videoconferences about this for 3 months andmthere are many aspects to take into account … How much will the vaccine cost? Will it cost the same everywhere or will there be a preferential price? How will we deal with the logistics of the distribution, with ultra-cold chains (at -80 oC) in countries where there is no electricity? … There is still a lot to decide, and there are many actors involved, but what we can never forget is that this epidemic does not stop with one country, it stops with everyone!
Here you can see the full interview (in Catalan).