The definitive solution to severe dysfunction of vital organs such as the heart, lungs or kidneys is to replace the damaged organ with a functional one from a donor. However, this is not a real option for many patients, due mainly to a lack of donors together with immune system incompatibilities. That is why scientists are looking for ways to make organs in the laboratory.
One strategy involves the 3D printing of organs from various cells and other components. Although this tool has great theoretical potential, it is still far from being applied to patients.
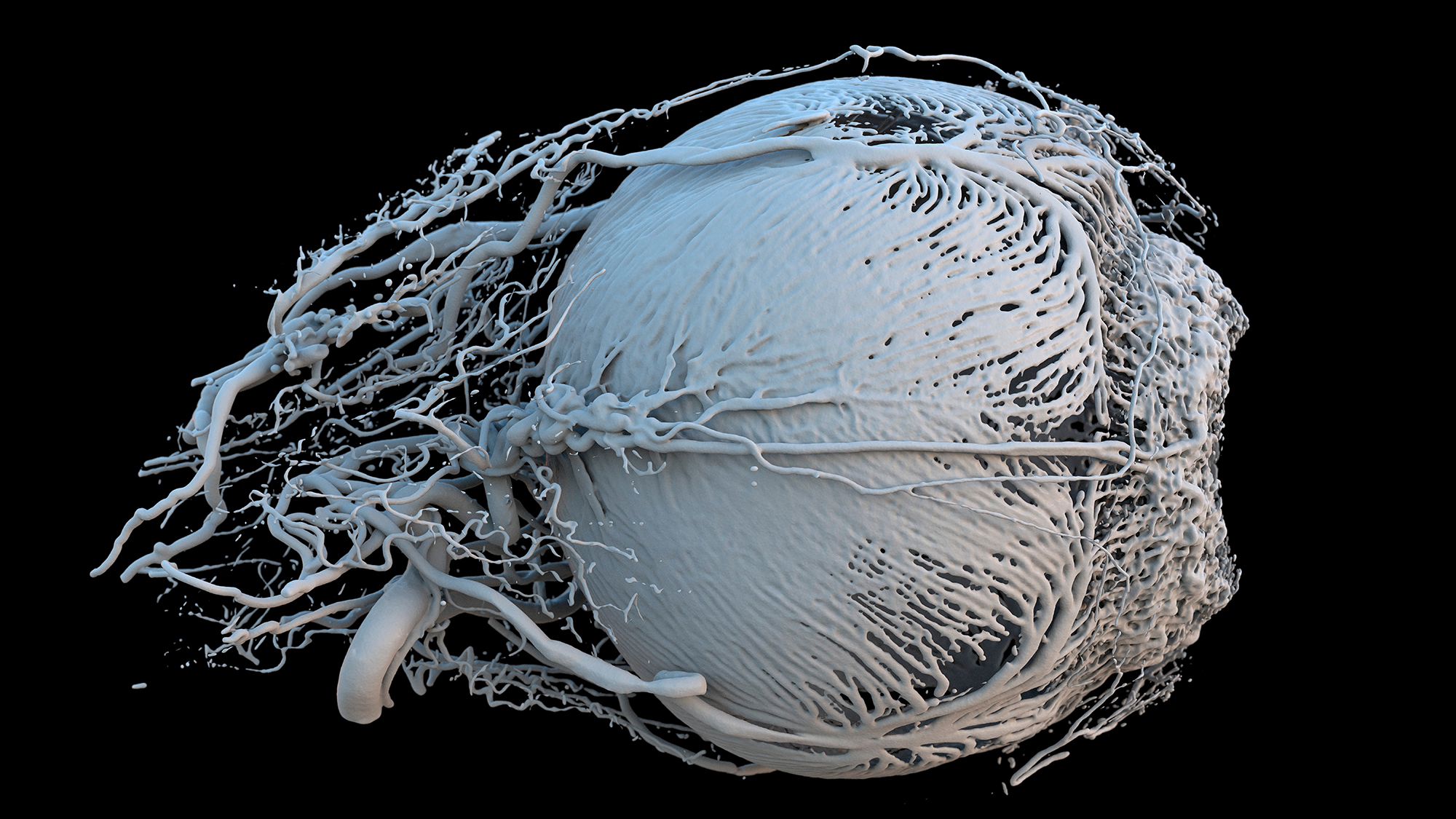
Instead, generating organs from an initial structure is a more realistic short- to medium-term option. Our organs comprise specialised cells (e.g. contracting cells in the heart, and oxygen-capturing cells in the lungs), which are spatially organised thanks to a structure made of proteins and other molecules, known as the extracellular matrix. It is possible to remove cells from the organs to leave only the extracellular matrix, and then refill this with cells that differentiate into specialised cells. Leaving only this structure and repopulating it with the patient’s own cells, avoids immune rejection problems. The use of artificial extracellular matrices or those of animals is also being investigated as a way of increasing availability.
It is possible to remove cells from the organs to leave only the extracellular matrix, and then refill this with cells that differentiate into specialised cells
These techniques have been already applied to patients to repair organ fragments with simple structures, such as the bladder or the respiratory tract. However, for entire organs with more complex structures, the protocols must be optimised and ensure long-term functionality. It is expected that diseases which are currently fatal will cease to be so in the coming decades.