It was 40 years ago that Luc Montagnier’s team at the Pasteur Institute in Paris published the first paper identifying the HIV virus in Science. Only two years had passed since its clinical description. Three years after that paper, in 1985, Simon Wain-Hobson and four other scientists succeeded in sequencing the virus. Soon after, Wain-Hobson set up his own laboratory.
In 1988, Andreas Meyerhans, now an ICREA research professor at the Department of Medicine and Life Sciences (MELIS-UPF), began his HIV research in the newly established Wain-Hobson laboratory. A chemist by training, Meyerhans had done his PhD in biotechnology, where he studied translation control in bacteria. Fascinated by Wain-Hobson’s enthusiasm, he decided to do his postdoctoral research in his laboratory. This was the beginning of a research career that has been closely associated with HIV for the past 35 years.
HIV currently infects 1.5 million people worlwide every year, and around 650,000 die of AIDS (Acquired Immune Deficiency Syndrome). Although much progress has been made since the first treatments and treated patients can currently lead relatively healthy lives, there is still no cure or protective vaccine for this chronic viral disease.
It was a very exciting time, not only in terms of scientific novelty
The story of HIV research is one of important scientific discoveries in the field of virology. But it is also a human story, of people and institutions fighting against the stigma of a disease associated with minority groups such as homosexuals and sex workers. Meyerhans recalls how, in the 1980s, this stigma affected the funding of scientific research and even led to demonstrations at virology congresses demanding more funding or free treatment. “It was a very exciting time, not only in terms of scientific novelty”, he says. On this subject, he recommends journalist Randy Shilts’ book, “And the Band Played On: Politics, People, and the AIDS Epidemic”, a chronicle of the scientific, social and political history of AIDS.
HIV drug developments
The first drugs developed prevented the virus from replicating by inhibiting reverse transcriptase, the enzyme that allows it to multiply. But patients developed resistance to the drugs and ended up dying from AIDS. Treatment did not progress until 1995, when antiviral drugs were developed that, in combination with transcriptase inhibitors, could reduce patients’ viral loads dramatically. This improved their health and reduced the likelihood of transmission.
Over the decades, treatment has been improved by defining more viral targets, and HIV infection has become a chronic disease. Today, treated patients live healthy lives and have a life expectancy almost as long as uninfected people. However, they still need to take constant medication to prevent the virus from reappearing. Some research groups are working to improve these drugs so they need not be given so often, improving these people’s lives.
There can be as much HIV variability in a single person as there is influenza virus variability in an entire population
Work is also continuing on a preventive vaccine and a cure for the infection.
The main difficulty in developing a vaccine is the high variability of the virus, which Meyerhans identified in his first article on HIV in 1989. “There can be as much HIV variability in a single person as there is influenza virus variability in an entire population”, he says, due to the rapid virus turn-over in vivo and its high mutation rate.
In terms of a cure, one of the key problems is the latency of the virus, which allows it to evade antiviral drugs and the immune system. Meyerhans explains that the balance between production and destruction of the virus in the body is a key area of research. It represents the constant fight between an expanding virus and the virus-restricting immune response.
The dynamics between HIV and the immune system
After leaving the Pasteur Institute, Meyerhans returned to Germany and established a line of HIV research that he has continued to this day. He came to Barcelona and the Barcelona Biomedical Research Park (PRBB) for love – and stayed, in love also with the kind of research he could develop here.
At the PRBB, he found a variety of scientific and technical services that opened the door to new questions. He has been able to work with different centres that have given him different perspectives on the subject he is interested in: the dynamics established between the virus and the immune system. For example, he has been able to carry out studies at the microscopic level with the Centre for Genomic Regulation (CRG), or to work with researchers at the Hospital del Mar Research Institute, who have provided him with interesting questions at the clinical level. He is also currently working with the European Molecular Biology Laboratory – Barcelona (EMBL Barcelona) at the mesoscopic level, looking at what happens at the organ level.
Meyerhans’ team takes a systems-level approach, focusing on the dynamics of the immune system, and has been interested in questions such as: what distinguishes an acute infection from a chronic one; how virus production and clearance are balanced in a chronic infection; what traces are left in our bodies after an acute infection; how these processes differ from those that occur during vaccination; or how we can get rid of latent – or dormant – viruses.

His conceptual interest in the dynamic process of chronic infection has also led him to collaborate with scientists from other fields, such as the mathematician Gennady Bocharov from Russia’s Marchuk Institute of Numerical Mathematics. Together, they have developed a model that can facilitate the design of vaccines, predict the immune response to an infection and determine the threshold of immune cells needed to fight it.
Latest progress towards a cure
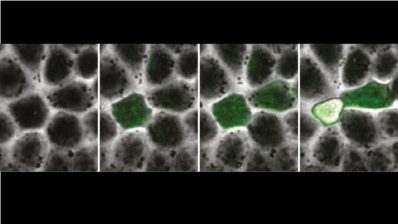
The latest publication from Meyerhans’ group provides new data on latency, a key aspect in advancing cures for chronic infections such as HIV. In an international study led by Meyerhans and Juana Díez, also of MELIS-UPF, they identified a new restriction factor called Schlafen12.
Schalafen12, which means “sleeping” in German, is a protein that restricts the production of viral proteins. It puts the virus to sleep, but also allows it to hide from antiviral drugs and the immune system. This makes it an attractive therapeutic target. In theory, blocking it could lead to an increase in viral proteins, allowing the immune system to ‘see’ the virus and eliminate it more efficiently.
HIV research: beyond AIDS
Meyerhans finds HIV research interesting because “it gives us fundamental knowledge on many levels: molecular, immunological and medical”, about how chronic viral diseases beyond AIDS work. Understanding the mechanisms that regulate the balance between infection and immune response is indeed key to many chronic diseases, such as AIDS but also hepatitis. Studies by Meyerhans’ group, like the one on dendritic cells that reactivate the immune system when it is exhausted from fighting an infection, are revealing new therapeutic targets for chronic viral diseases or even cancer.
Thus, studying the dynamics of the immune system in the face of an infection such as HIV can help us to understand important aspects, including the chronification of an infection, drug resistance or which drugs can be combined. For Meyerhans, it is all a question of balance. In this dance between the virus and the immune system, it is all about “being in the right place at the right time,” he says.
It is important to ask risky and wide questions, because along the way we understand what we need to do
The researcher recalls a project in which they tried to develop a universal vaccine for chronic infections and, although they did not succeed, they learned a lot in the direction of functional cure strategies. “It is important to ask risky and wide questions, because along the way we understand what we need to do,” he says.