Marc Güell studied a degree on chemistry followed by telecommunications engineering. After his PhD at the European Molecular Biology Laboratory (EMBL) and the Centre for Genomic Regulation (CRG), he left for Boston, to Harvard University’s Wyss Institute, where he started developing new technologies for gene editing and synthetic biology. Since the summer 2017, he has led the Translational Synthetic Biology research group at Department of Experimental and Health Sciences, Pompeu Fabra University (DCEXS-UPF), where he is working to apply advances in genetic engineering in therapies.
You came back from Harvard to set up again in Barcelona. Why?
I feel very European and I wanted to come back here. The quality of science in Barcelona is very high. Perhaps we stand out more for basic research, but even so, there are all of the ingredients to do very good research and the city attracts international talent. I’ve had a chance to go to other places, but I wanted to come back.
“(In Barcelona) there are all of the ingredients to do very good research and the city attracts international talent”
Marc Güell
What differences have you noticed between research in the United States and here?
The price of failure in the United States is far lower than here, the Americans are very risk-oriented. This allows them to come up with findings that we find harder to do in Europe. It is true that many high risk projects end up failing, however, often, the great discoveries come from this type of projects. These initiatives, in Europe, often have difficulty finding funding.
You studied chemistry and telecommunications engineering to end up dedicating yourself to synthetic biology.
I’ve always liked the experimental science and technological development. I could have done any experimental sciences degree. Then telecommunications gave me my training in computing. In the end, I ended up doing synthetic biology because I really like to create technologies that allow us to solve problems. And as living matter is the most advanced machinery that exists, I was aroused by the challenge of doing engineering in living systems to create new therapies.
“I really like to create technologies that allow us to solve problems”
How does gene therapy work?
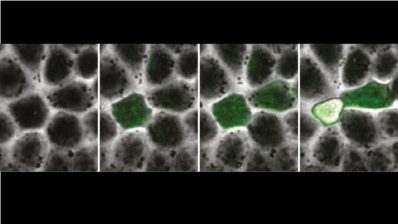
There are two ways. One is the ex vivo method, where you extract an entire tissue, it is genetically modified and, once it works properly, it is re-introduced. In the case of bubble children, haematopoietic cells are taken from them, these are genetically modified and re-introduced. In other cases, this option is not feasible and the genetic material of interest must be introduced to the cells without removing them from the body. Then we work with viruses or other nanoparticles that can introduce the genes into the cells of the tissue.
In addition to your research, you have created the eGenesis spin-off. How did that come about?
During my stay at Harvard, I was dedicated to editing the genomes of mammalian cells. We made quite some progress and we asked ourselves how we could materialize our findings to solve a major medical problem. The lack of tissues for transplantation is one of the biggest current medical problems and it seems not to have an easy solution: we are becoming increasingly old and we are better at keeping critically ill patients alive, so there are few prospects of increasing the numbers of organs available for transplantation. One possibility to produce unlimited organs is to use animals, such as pigs.
What difficulties does this process involve?
A priori we have to break two barriers: compatibility with our immune system and endogenous viruses. Virtually all mammals have within their DNA endogenous viruses that are transmitted from parents to offspring. In the case of humans, we take hardly any notice of them because they are ancient and are practically inactive. But not in the case of pigs; they are a more recent acquisition and can infect human cells. As we are dealing with endogenous viruses, no matter how clear we keep our cells, viruses will continue to be transmitted. The only solution seems to be to apply genetic engineering to make more compatible animals without active endogenous viruses.
“Gene therapy is already a reality (…), but in long term, it will generate much debate”
What are the main implications of your findings?
In the short and medium term, we are working to create tools that will allow us to cure diseases. Gene therapy is already a reality: its use to treat leukaemia, joining a growing list of diseases, has just been approved. But in the long term, it will generate much debate. The importance of modifying the human species in a targeted fashion has implications that go beyond the labs.
“The research we carry out only means something if it reaches everyone”
Where is the limit?
We have to learn the limit as we go. At the moment, there is a broad consensus on the use of genetic engineering in somatic cells for therapeutic purposes (thousands of clinical trials in progress). However, recently the technical feasibility of modifying human embryos has been demonstrated. These modifications that affect the germ line will in all certainty take longer to come out of the lab.
Technology is progressing very fast and the debate is not only ethical, but there’s also a considerable economic component. When we have at our disposal a treatment for leukaemia but this treatment costs half a million euros, how will we manage it? In the end, the research we carry out only means something if it reaches everyone. This is not a decision to be taken by us scientists but it is important for us to inform that gene therapy has come to society to stay and to expand.