March saw the launch of the European ‘SkinDev’ project, coordinated by Marc Güell of the Department of Medicine and Life Sciences (MELIS). Its aim is to use synthetic biology to modify the skin microbiome that could, in the future, serve as a platform for developing therapeutic or diagnostic tools. The initial focus will be on atopic dermatitis, a chronic skin irritation characterised by dryness and eczema formation.
The project has received three million euros from the European Innovation Council, a body that seeks to identify, develop and scale up cutting-edge technologies and breakthrough innovations. In addition to UPF, teams from England, the Netherlands and Germany are participating, all led by young researchers.
We spoke with Javier Santos, postdoctoral a researcher in the lab led by Marc Güell at the UPF and a participant in the project.

What is the aim of this project?
Current treatments for dermatitis, mostly corticosteroid creams, have side effects and require constant application. Our proposal is to modify one of the skin’s natural bacteria so that it detects when there is irritation and releases anti-inflammatory drugs directly.
The aim of the project is to modify a naturally occurring bacterium in the skin to detect irritation and release anti-inflammatory drugs locally.
To do this, we propose to use Cutibacterium acnes, a bacterium that under normal conditions prevents other pathogens from infecting us. It has several advantages:
1- it is the most abundant bacteria on the skin, so our skin is used to having it in large quantities.
2- it is mainly found in the follicles, i.e. not in the most superficial part of the skin, but a little deeper, so it does not leave the skin so easily, for example when bathing, and instead it remains on the skin for longer.
In fact, a previous study from our lab showed that bacteria isolated from a donor person could be applied to a recipient person and remain there for several weeks. They then disappeared on their own, which is also an advantage.
So how do you put these bacteria on the skin?
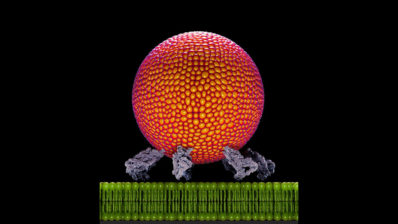
After making the necessary modifications so that the bacteria are able to detect inflammation locally and, in response, release the anti-inflammatory molecule we have added, they are grown and resuspended in a solution. The end product is a preparation (a liquid, or emulsion) with the bacteria in suspension. The idea is then to put a few drops on the skin, as if you were putting on cologne or a cream, and the bacteria enter the follicles on their own.
The bacteria would produce and locally release an anti-inflammatory molecule for the 2-3 weeks that the bacteria remain on the skin. If after that time you still need treatment, it could be reapplied. You could even think about putting the bacteria on every so often, as a preventive measure (not only when you see inflammation), and the bacteria would detect when the skin is becoming inflamed and stop the process from the beginning; and if there is no inflammation, then the bacteria would do nothing.
There are many possibilities… But until now almost nobody has been able to modify C. acnes, to control its behaviour. And this is obviously the first step.
And have you succeeded?
It was difficult to get external DNA to enter the bacteria to begin with, because they have several mechanisms to prevent it, such as restriction enzymes, or CRISPR. We have now managed to create DNA that escapes this attack by the bacteria.
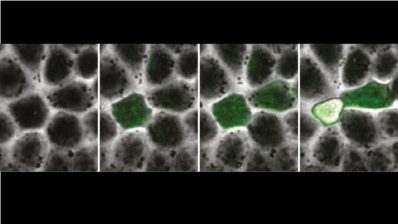
The next hurdle was to have molecular tools to modify this particular bacterium – the tools that already exist for other bacteria, such as GFP (the fluorescent protein that tells you whether a gene is being expressed or not) had not been tried with C. acnes. And we have also made progress on this; we are developing a kind of ‘toolbox’ to be able to modify this type of bacteria.
How long have you been working with this bacterium?
The lab has been working on this issue for about 5-6 years, although the last year is when we have made the most progress. You have to bear in mind that science is not linear, sometimes it takes a long time to overcome an obstacle, and then perhaps progress is made all at once. Another disadvantage is that this bacterium grows relatively slowly; just as E. coli can grow in one day, C. acnes takes a week.
But these recent advances, with which we have shown that it is possible to modify the bacteria, are what allowed us to obtain funding for this European project.
How is the project organised?
It has three main axes, which will be carried out by the different collaborators:
- Developing tools so that the bacteria can detect inflammation in cases of atopic dermatitis and fight it. This part is what we are doing mainly in our laboratory, and with Rodrigo Ledesma from Imperial College London.
- Creating mathematical models of atopic dermatitis that help in the development of bacteria, defining how many molecules are needed, identifying which are the most promising biomarkers of inflammation, or predicting how our modified strains interact with the skin and with the skin’s natural microbiota, for example. For this we have the team led by Reiko Tanaka, also from Imperial.
- Developing 3D cell cultures (a kind of skin ‘organoid‘) to test the newly created C. acnes strains. This part is being carried out by Ellen Van den Bogaard of the Radboud Medical Center University in the Netherlands and Bernhardt Homey of the University of Düsseldorf.
So the functional tests will be done in vitro?
There are mouse dermatitis models, but I don’t know to what extent our results could be extrapolated, because mice don’t naturally have C. acnes. So for the moment we are going to test the functionality in human cells in 3D culture, which would be the closest thing.
In any case, the last step would be a clinical trial in humans; but the way we are doing the project now, it would not be possible, because we use antibiotic resistance to select the bacteria we want, and so on. This is fine for rapid progress, but for clinical use we would have to use something else, and we are already working on that. In any case, nowadays it is difficult in Europe to get a trial with modified bacteria approved… it generates a bit of suspicion. In the US there are already some clinical trials with this type of bacteria, but in Europe the control is more restrictive.
If this works, could these bacteria also be modified to treat other diseases or conditions?
Yes, right now Nastassia Knödlseder in our lab is already working on acne and hair loss.