The placenta is a key organ in development that evolves during pregnancy and regulates nutrient, oxygen and waste exchange between the maternal blood and the fetus. Therefore, the development of a healthy placenta is key for the proper growth of the fetus and to preserve maternal health.
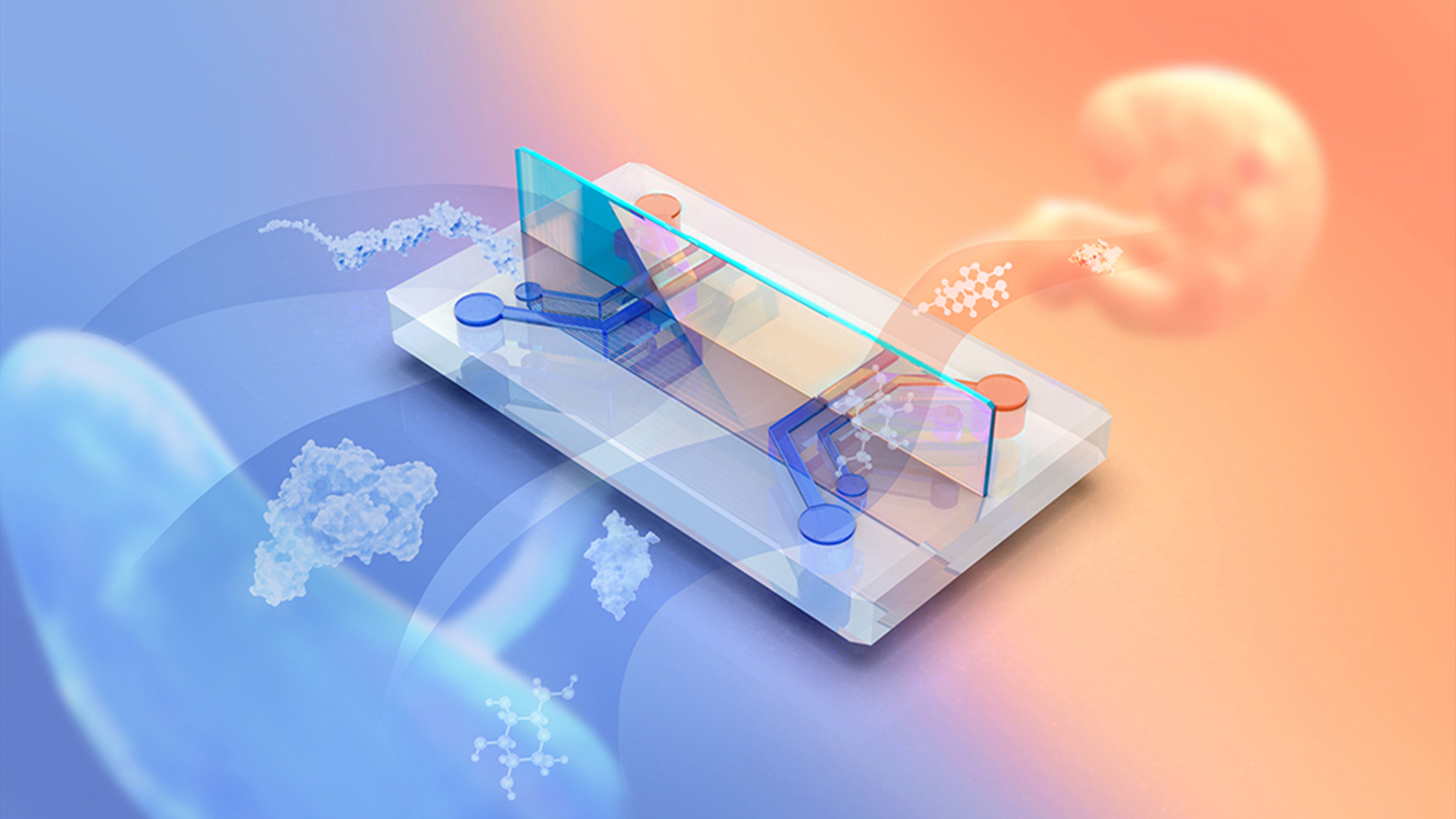
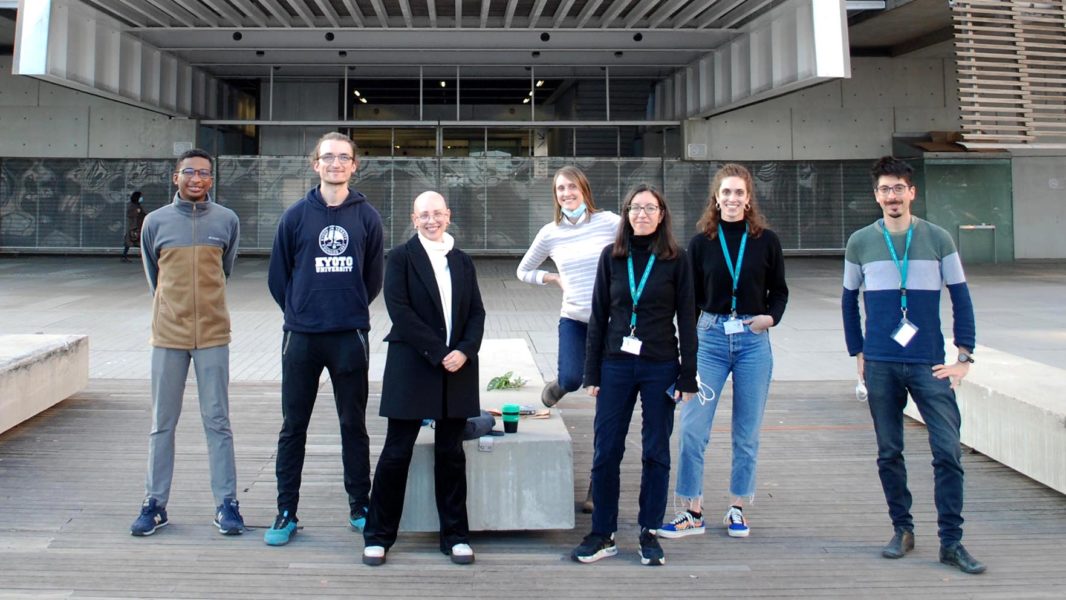
In a pioneering model, Marta Cherubini, a postdoc at the Haase lab at the European Molecular Biology Laboratory – Barcelona (EMBL Barcelona), has been able to produce, in a chip, fetal vasculature similar to that from the chorionic villi – the terminal branches containing fetal vessels which interface with trophoblastic cells, where the exchange of substances with maternal blood occurs.
A multicellular, perfusable and reproducible system
To recreate the fetal vasculature, they cultured endothelial and stromal cells derived from the umbilical cord and placental explants inside a flexible device. “We can now culture these microvessels for 21 days but we expect to increase this time by culturing them under continuous flow as would exist in vivo”, says Cherubini. An improvement enabled by their main expertise: generating perfusable vessels, something that is essential for the viability and proper development of the organ.
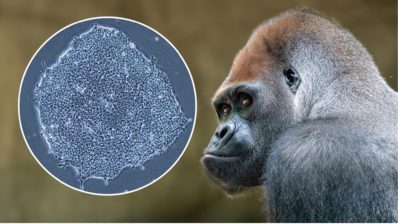
Besides, this 3D in vitro system will be more reproducible than an explant tissue that rapidly degrades outside of the body. And, contrary to existing models developed with animal cells, it will mimic the physiology of the human placenta. Therefore, they will fill the gap by proposing “a relevant model for researchers and pharma companies to study placental development and test whether selected substances actually pass through the placental barrier”, notes Kristina Haase, leader of the project.
The 3D in vitro system developed by the lab will be a relevant model to study placental barrier function and test which substances pass through the placenta and how they do it.
Partners to combat placental diseases
Preeclampsia is one of the most common placental dysfunctions. Its cause is still unknown but it is concomitant with maternal high blood pressure and inflammation. To better study the disease, the Haase’s lab has established a collaboration with Dr. Elena Carreras and Dr. Manel Mendoza from Vall d’Hebron hospital in Barcelona. They plan to collect either serum of pregnant women suffering from the disease to see its effect on a healthy system, or cells from preeclamptic placenta to recreate affected vessels.
In both cases, the scientists expect to better understand the changes in the placental barrier induced by preeclampsia. In addition, and thanks to their perfusable system, they plan to test existing and new drugs to subside disease effects.
Besides, they will also study the effect of pregnancy-specific glycoproteins (PSGs), produced by the trophoblast, in preeclampsia. One of the PSG proteins, PSG1, is related to vascular viability and development and its levels decrease upon disease. For this study, they will collaborate with Professor Gabriela Dveksler from the Uniformed Services University of the Health Sciences in the United States.
A system with a promising future
Although they are still refining the barrier function of the system to limit all substances larger than 1kDa, Cherubini and Haase believe that this 3D placenta on a chip has a brilliant future. “Our long term goal is to use this system to test the toxicology of substances transitioning from maternal blood to the fetus. Right now there is no relevant model for companies to test whether their drug actually passes or not through the placental barrier”, states Haase.
That is why they believe that this multicellular device will pave the way to test the compatibility of food substances, such as caffeine, or drugs with a healthy pregnancy. Taking into account the key importance of the fetal exposures to the child and adult health, this system may prove of extreme practical relevance.